By Paul C. Waldeck, B.Eng. (Hons.) C.Eng. MICE. MIStruct.E. MIMechE. MASHRAE, Technical Director, PPL-Biosafety International
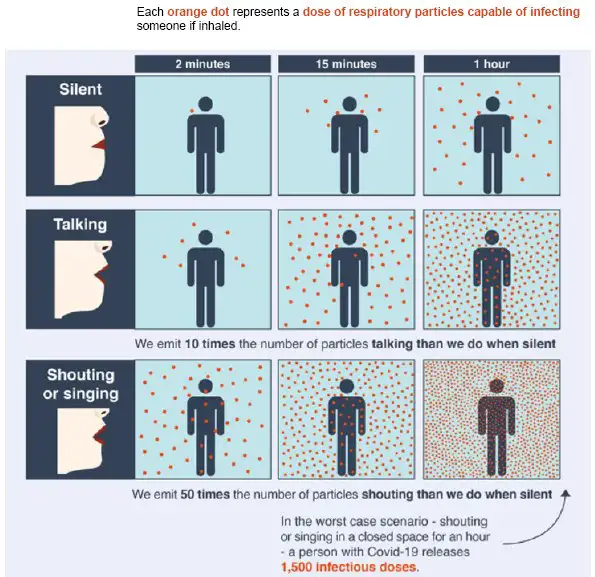
The coronavirus pandemic has brought a widespread understanding that interior spaces have the power to make us sick or keep us well (Figure 1). This virus primarily is an airborne infectious pathogen, and so, breathing in contaminated air could lead to COVID-19, with both the short- and long-term harm it brings.
Interior Air Quality (IAQ) has been high on the agenda of regulators around the world. Now, COVID-19 has helped to accelerate the changes that value the quality of the air that we breathe as important to health as the water we drink.
The American Society of Heating, Refrigerating, Air-Conditioning Engineers (ASHRAE) has been at the forefront of calling the pandemic correctly. In April 2020, “ASHRAE Position Document on Infectious Aerosols” grabbed the attention of scientists, engineers, medics and policymakers around the world, but it took over a year for the Centers for Disease Control and Prevention (CDC), Environmental Protection Agency (EPA), World Health Organization (WHO) and governments around the world to assert that ventilation was a key pillar to infection prevention and control.
The use of recirculated air in building HVAC systems is commonplace because it is energy efficient. After all, who wants to draw in outside air, heat it in winter or cool it in summer, pass it through the building and then throw it away after that first pass? In the challenging times of energy crisis and cost of living increases, I doubt there are many who are prepared to be so wasteful, even if it weren’t for the pandemic and risk of infection.
Recirculating air is cost-effective but not helpful to bio-risk reduction if one is recirculating and resharing potentially bio-contaminated air. So, what are regulators and institutions saying? In the US, one can use recirculated air if it is passed through a MERV 13 filter, or the air is cleaned or disinfected by germicidal UV-C (aka UVGI).
The increasing of filters is not always sustainable or practical for the HVAC plant because the plant might need upgrades to allow it to push that air through much tighter filter pores. Another challenge is that many experts are recommending six air changes per hour for ventilation standards, plus the use of these these higher filter grades to create safer, less bio-hazardous air to breathe. Again, the energy and plant capacity challenges apply. One keeps returning to the need for UVGI in the HVAC system because it enables normal filter sizes and disinfects the air using low amounts of energy.
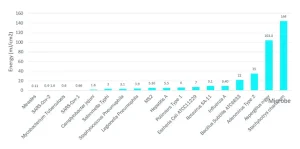
UV-C air disinfection has been highly effective against the transmission of measles, probably one of the most infectious diseases known to mankind, as well as other airborne pathogens and diseases such as tuberculosis, SARS-CoV, RSV, Aspergillus and Influenza A, to name but a few. This effectiveness extends to most all other bacteria, fungal spores and viruses, too. Indeed, it takes only very tiny amounts of energy to inactivate viruses and bacteria, as illustrated by Figure 2.
Europe has been updating its ventilation regulations and. in June 2022, the new English Building Regulations Part F – Ventilation became mandatory:
Recirculation of air within ventilation systems in offices
1.37 Ventilation systems that, under normal operation, recirculate air between more than one space, room or zone should also be able to operate in a mode that reduces the risk of the transmission of airborne infection. This can be achieved by one or more of the following.
a. Systems capable of providing 100% outdoor air to the levels specified in paragraphs 1.32 to 1.34 to all occupiable rooms and common spaces, without recirculating air.
b. Systems incorporating a UV-C germicidal irradiation system that is able to disinfect the air that is being recirculated. This type of system is commonly located within the heating, ventilation and air conditioning (HVAC) system or ductwork.
c. Systems designed so that they can incorporate HEPA filters if required, which are able to provide filtration of the recirculated air.
This essential amendment was instigated by the UK government’s Scientific and Advisory Group for Emergencies in response to airborne pathogens such as COVID-19, as well as the group’s concern over influenza pandemic risk and other airborne infection epidemics or pandemics in the future.
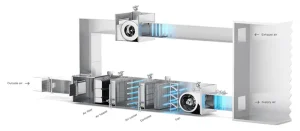
The aim is to create pandemic resilience against airborne respiratory diseases within the built environment by improving ventilation, filtration and adding air disinfection systems for new and existing buildings, whilst mindful of low carbon targets. It is economical and safe to recirculate air back into rooms when UV-C systems are designed by competent and qualified professionals.
PPL-Biosafety designs and supplies lamps for HVAC UVGI infection prevention and control systems for clients around the world. It has come as a shock to see how poor some ventilation systems are, even in buildings in which higher levels of protection would be expected. If there has been one good thing about COVID-19, it is that regulators have come to grips with the importance of adequate ventilation and how old technology, like UVGI, can be retrofitted easily into existing buildings and transport systems to make spaces safer.
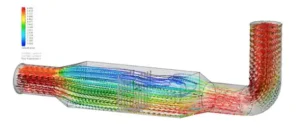
The new regulations in Europe, the UK or the US are not prescriptive on how to design a competent UVGI HVAC solution. Complex computational fluid dynamics (CFD) modeling of the duct systems is recommended because the mathematics are heavy across a great many design parameters.
ASHRAE Handbook’s “Chapter 62: Ultraviolet Air and Surface Treatment” currently is being updated to reflect what has been learned during the pandemic. It likely will be a great resource for professionals in the sector when it is published in mid-2023.
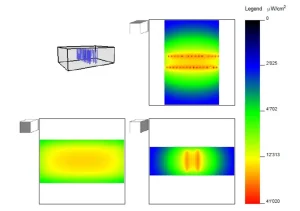 Qualified professionals assess a range of scenarios when designing and building HVAC systems for UVGI upgrades. Typically, they look at Influenza A as the target microbe to disinfect to between Log-2 (99%) to Log-4 (99.99%) reduction on the first pass of the air past the UVGI array. This should provide a significant factor of safety against coronaviruses, which are easier to destroy by a factor of 3. Typical
Qualified professionals assess a range of scenarios when designing and building HVAC systems for UVGI upgrades. Typically, they look at Influenza A as the target microbe to disinfect to between Log-2 (99%) to Log-4 (99.99%) reduction on the first pass of the air past the UVGI array. This should provide a significant factor of safety against coronaviruses, which are easier to destroy by a factor of 3. Typical
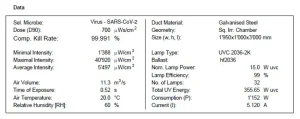
calculation output is shown in Figure 5.
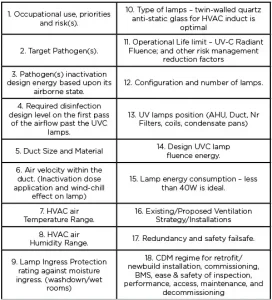
While for now the regulators are not being prescriptive, one must take great care to ensure that one designs and models accurately to a factor of safety that will represent real-life use. Key factors to consider are detailed in Figure 6.
In conclusion, regulatory changes that support the use of UVGI to create more “immune” buildings are welcomed. The UVGI market needs to be ready to service the increased demand, and this also means increasing resources with professional, qualified and competent people who know how to deal with infection prevention and control using engineered biosafety solutions.
A golden opportunity now exists for progressive private and public sector entities to embrace best practices from around the world to improve IAQ and build bio-defenses with better ventilation and professionally designed UVGI. This will protect their workforces, which means not just a compliance tick but happier, healthier staff who are safer. This, in turn, creates a business that is less prone to operational disruption from increased sick days or super-spreader events. And, above all, it will create a pandemic-resilient business that is ready for whatever the future may bring.
Paul C. Waldeck is the technical director at PPL-Biosafety International. For more information, email paul.waldeck@ppl-biosafety.com or visit www.ppl-biosafety.com.